BHG Activates Cares Disaster Plan in Wake of Hurricane Ida
By Jay Higham, CEO
[insert branded Disaster Care Response Plan graphic]
As Hurricane Ida left her path of destruction, all of those affected by this tragedy weigh heavy on my heart. Hurricane Ida rapidly grew in strength before hitting the coast of Louisiana and made its way through much of our Behavioral Health Group (BHG) locations affecting our team members and our patients. Among the chaos, the storm left behind structural damage, flooding and loss of power. Ida displaced families and destroyed homes and businesses. Employees, patients and communities continue to struggle as they come to grips with the devastation caused by the storm.
We are so proud of our dedicated team members, who while dealing with their own struggles, have remained committed to supporting our patients. By the Saturday following the hurricane, team members who could get into the city came to our centers so we could open for patients who needed dosing. Many of our team members had yet to assess the damage to their own homes, but they returned to help our patients. BHG will forever be grateful for their dedication and perseverance.
We’ve activated our BHG Cares Disaster Response Plan. This means that BHG is supplying water, non-perishable food items, toiletries, and financial and emotional support to affected employees. It was a true team effort with our emergency preparedness plans and so many of our teams across the country went into action, doing what they do best, supporting our BHG work family and taking care of business.
Many of you continue to ask how you can support those affected. You may consider making a voluntary donation to government supported resources such as:
I couldn’t be more proud of our teams and we are here for our New Orleans team members and patients as they go through the process of rebuilding their lives and homes following this detestation.
BHG Pilots Customizable SAMMS in Knoxville
By Rebecca Hardman, PMP, Director of Project Management and Clinical Informatics
Imagine a day when patients do self-check-in with their ID cards at a kiosk across from your front desk. Their name appears on the screen along with personal information, including insurance, billing and history. They review and update their file, and after the appointment, the counselor enters notes and a claim is automatically generated for the provider. If it’s cash pay, an invoice is created for the patient. By the next appointment, if payment is still due, the patient pays at the kiosk. When the compliance team needs information, RCM reports are due, or any metrics are requested, everything you need is in SAMMS (substance abuse medication management system). No more filling in paper forms that are housed in file-cabinet-filled rooms or incorrect data that interferes with RCM. No more long lines and frustrated patients. Most importantly, staff have more time to focus on patient care.
This is the goal for all BHG treatment centers.
This summer, our Clinical Infomatics team has worked diligently to start us down this path by piloting a new, customizable version of SAMMS V6 at our OBOT in Knoxville, TN, where up until September, they were completely paper-based.
One of the primary drivers for doing this is to meet the increasingly complex standards that our payors are requiring. While some centers have SAMMS V6, it’s not the same as what we’re doing in Knoxville. When we were considering a new software vendor, leadership challenged our current one to meet our needs for consistency across all centers with the ability to customize data fields that differ by payors state by state. This is giving us the quality documentation that will allow us to meet those expectations.
Knoxville, the model for all BHG centers
The new version of SAMMS is more intuitive and includes significant updates that will make all of our lives easier in the long run.
- Higher quality data entry and reporting
- Standardized, repeatable process and work flow
- Allows check for insurance eligibility
- Ability for patients to complete paperwork at home before appointments
- Improved clinical documentation that is stored in a more traditional database and can be queried and checked for quality assurance
- Use of the “Golden Thread” data concept – enter something once and it carries through the system so it doesn’t have to be entered anywhere else again.
- Ability to do more auditing, a huge benefit to the compliance team
- Provides more metrics and statistics for the RCM system, making payors more willing to pay us
- Improved patient experience with self-check-in kiosks
- Frees up time for patient registration, call center and front desk to do their jobs
- Know who does and doesn’t have insurance via color-coded appointment calendar
- Improved documentation for group sessions where all patients show up on the group roster and counselors can enter notes on individuals’ files
Over the last month, we’ve entered patient data and the clinical informatics team has defined processes, tested software and conducted go-live training. At the end of September, we’ll follow up and assess what we’ve done with the OBOT and determine how much of that carries over to revamping our OTPs. While we don’t have an exact timeline, we’re moving through the OBOT pilot fairly quickly and will move into an OTP pilot. Once the pilots are done and leadership is comfortable, we’ll roll out the customizable SAMMS nationwide.
Perspective from the Knoxville team

“When I started in January, I was a little startled that we still used paper,” said Tiffany Vargas, Director of OBOT Services – Tennessee. “This pilot has been a journey and a little bit of a whirlwind. Given that we were completely paper based, our staff are very excited to transition into the modern world of an EHR. It’s nice to have a lot of input into the new system. We’re making recommendations whenever we see things that don’t work quite right or make sense. We’re seeing updates literally every week and we’re trying to optimize this opportunity as much as we can. The Clinical Informatics team has been amazing. They’ve provided trainings, created tip sheets for our staff to reference back to and hopped on ZOOM sessions to trouble shoot when we run into issues. The tip sheets are a lifesaver and will be the templates they’ll use to educate across the company.”
“We’re now working on using the self-check-in kiosk, which patients are responding well to. We’re in the process of getting all of the supplies, taking pictures, and printing the patient IDs so that the patients can use the kiosk independently,” said Tiffany.
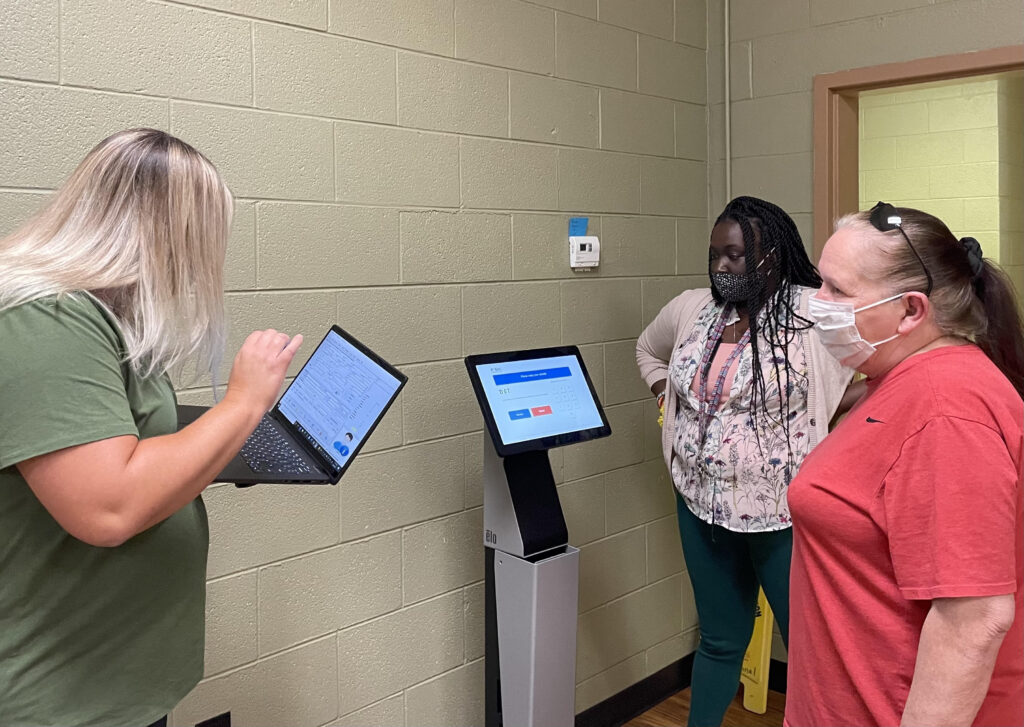
Regional OBOT Director, Tiffany Vargas (left) and Counselor Kendra Coger (right) helping a patient check-in via the self-check-in kiosk that will be used for all group check-ins at Medical Services – Knoxville. 
Below is a picture of our 1st patient learning how to do self-check-in from Group Counselor Kendra Coger for the Evening Recovery Group on Thursday, Sept. 9th. He was excited to see us implementing new technology and he and his wife said to make sure everyone knew that they think Kendra is awesome and they look forward to coming to her groups. 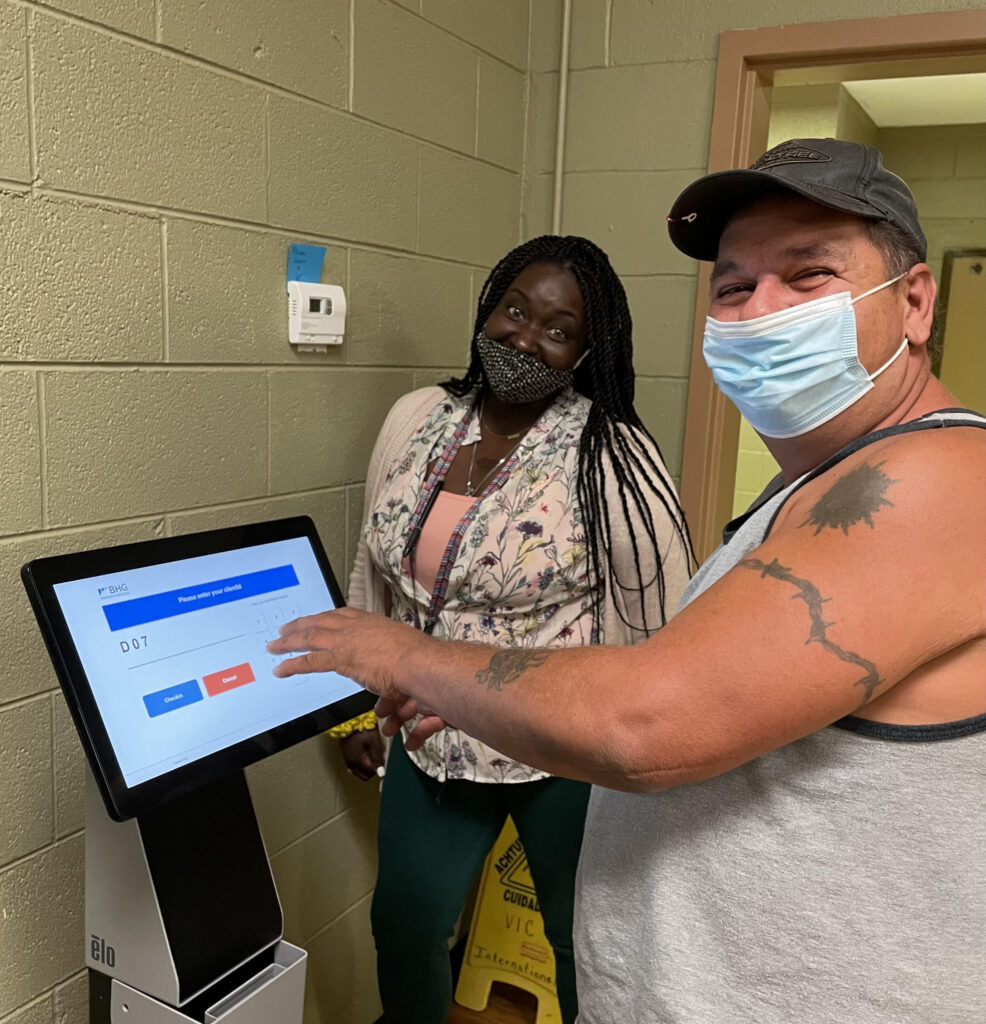
Counselor Kendra Cooper and a Medical Services – Knoxville exploring the new self-check-in process as part of the SAMMS V6 upgrade
“I’m a data person through and through,” said Tiffany. “My biggest concern here has been gathering data. It takes an insane amount of time to go through charts to find what you need when the State or payers request patient data. This updated SAMMS will make gathering that information more efficient with respect to time and manpower and it broadens the access points. Now when we have a request, our RCD can access our patient charts remotely. The new V6 of SAMMS will also make reporting for quality measures feasible as it can pull data together across patient charts to allow us to see if we’re making an impact. That helps us to institute best practices and evidence-based treatment in a way we couldn’t monitor before.”
“The ability to pull reports is probably my favorite feature though. As an example, OBOT doctors have a mandated patient cap which is something we have to monitor closely” Tiffany explained. “We’ve been using a grid on a whiteboard, the old-school way. This new system will replace that. We can go in at any point in time and enter the parameters and pull a report with the click of a few keys. The scheduling system is another example of that. We’ve created a color-coded status for calendar appointments to tell us where patients are in the verification process, if their insurance has been verified or not, if they are checked in, checked out, canceled, rescheduled or no-shows. We can run reports by provider and patient.”
“Here, patients can be in an OBOT, IOP or psych program and this system can query how many patients we have in these different programs in only a few minutes versus going through file cabinets and writing all of the names down.”
“While the change has been hectic and painful at times, all the change is and it will be worth it,” said Tiffany. “It’s important to keep an open mind. It’s all about letting go of the old way and learning the new way. It’s wonderful to go through this transition and growth from scratch. The staff look forward to the future and are already starting to see the benefits of all the hard work we’ve put in during this pilot. When you approach it from the 10,000-foot view of where will take us, it’s easy to be excited about what the system will do for us and our ability to further our mission of helping patients find recovery.”
