By Dr. Benjamin Nordstrom, Chief Medical Officer
Over the last five or so years, one of the most potent killers known as fentanyl has infiltrated the opioid mix and addiction crisis, adding to the complexities of our jobs to help save people’s lives. Some people willingly choose to take fentanyl, while others unknowingly ingest it through pills or other drugs laced with remnants left on scales by dealers who give little thought to the safety or well-being of drug users. To continue being a part of the solution, we must increase our understanding of this agent and ensure that protocols are established and consistent across all our BHG treatment centers.
Last month, the CDC released the staggering news that more than 93,000 souls lost their lives to drug overdose in 2020. That’s a 30% increase from 2019. Roughly 70% of those deaths involved opioids, many of which contained fentanyl. Between 1999-2019 we had 841,000 drug overdoses.[1] Since 1999, this country has lost more lives to drug overdose than it has lost in all of our foreign wars combined.*
Many of you attended the two Town Halls I led this month, but I encourage you to keep reading as a reminder of key points and how to best assist colleagues to understand fentanyls, especially as we fully implement the IDCM and support patients during the ebbs and flows of their recovery journey. For those of you not in clinical roles, I hope this information further sparks your passion for being a part of our team and the fight to help people recover from addiction. You can view the Town Hall presentation here.
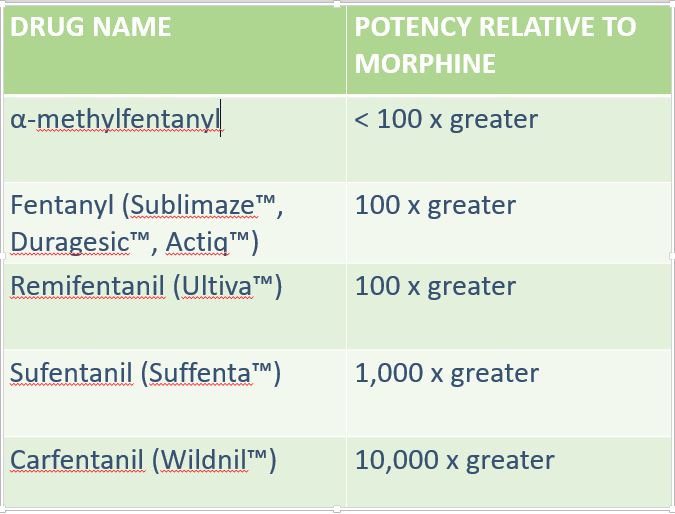
Fentanyl is 50 to 100 times more potent than morphine.
Fentanyl is a powerful synthetic opioid that is similar to morphine but is 50 to 100 times more potent. It is a prescription drug that is also made and used illegally. Like morphine, it is a medicine that is typically used to treat patients with severe pain, especially after surgery. In its prescription form, fentanyl is known by such names as Actiq®, Duragesic®, and Sublimaze®. When prescribed by a doctor, fentanyl can be given as a shot, a patch that is put on a person’s skin, or as lozenges that are sucked like cough drops. The illegally used fentanyl most often associated with recent overdoses is made in clandestine labs operated by narcotics syndicates. This synthetic fentanyl is sold illegally as a powder, dropped onto blotter paper, put in eye droppers and nasal sprays, or made into pills that look like other prescription opioids. Some drug dealers are mixing fentanyl with other drugs, such as heroin, cocaine, methamphetamine, and MDMA. This is because it takes very little to produce a high with fentanyl, making it a cheaper option. This is especially risky when people taking drugs don’t realize they might contain fentanyl as a cheap but dangerous additive. They might be taking stronger opioids than their bodies are used to and can be more likely to overdose.[3]

Assessment Summary- DEA Strategic Intelligence Section
When we’re talking about fentanyl, we should use the plural form, fentanyls, because there are multiple variations with different strengths.
What you need to know about lab testing for fentanyl
No FDA-approved point-of-care (Readi test) exists for fentanyl. One of the reasons we changed to Cordant was because they have fentanyl on their panels. But, we still have a two-step process: qualitative/ screening (EIA) – 98% true positive rate – and quantitative/ confirmatory (GCMS).
If a patient tests positive for fentanyl and for ANY other drug, do not send for confirmation. At most, there’s a 3% chance the test is wrong. They could easily have been exposed through contaminated drugs and it’s important to educate them on how common this is.
If a patient tests negative for fentanyl and all other drugs AND you believe the test may be incorrect, then send for confirmation.
It’s important to know that the EIA will likely turn positive for ANY fentanyl, but the GCMS will only give a result if plain fentanyl is there (and won’t be positive if they used something rarer like carfentanil, the most potent form of fentanyl). The other forms of fentanyl are less common on the street, but they are in circulation, so it’s important for us to bear this in mind.
Whether the exposure is purposeful or accidental, the patient is still in a dangerous place and we need to reduce their code and increase their program structure. It’s important that we help patients know that this is NOT A PUNISHMENT, but a way for us to address and monitor their health and safety. We should also strongly consider increasing the dose of medication they are receiving. If benzodiazepines or alcohol is also present, the risk of increasing the dose has to be balanced against the risk of continued use of fentanyl, and these situations are clinical challenges.
What we must do
Know treatment protocol for fentanyl-positive patients. Study the treatment details in my Town Hall presentation and take a deeper dive into the science by exploring the source links I’ve provided.
Education will not scare patients into not using fentanyl. While it’s important to continue informing our community partners and resources on what fentanyl is, how to recognize when someone may be using it and where to send patients, our job as clinicians is to integrate motivational interviewing and CBT as part of treatment. Some of you are certified in EMDR and have said you will consider utilizing this with patients. If you are lacking certifications and training or just have questions, talk to your Program Director about what steps to take next.
Hold fentanyl-positive patients tighter. When someone is using fentanyl, we must put our arms around them tighter, hold them closer and do more for them; not think of ways we can get rid of them. We are what’s good for them. We are what’s going to keep them alive.
As always, please reach out with questions, suggestions and concerns. We are in this together. Contact me at [email protected] or 603-306-6047. And, please continue to stay informed about COVID-19-related updates on our website.
*CHART: How Many Soldiers Died in Each U.S. War? | KQED
[1] https://www.cdc.gov/drugoverdose/deaths/index.html
[3] NIDA. 2021, June 1. Fentanyl DrugFacts. Retrieved from https://www.drugabuse.gov/publications/drugfacts/fentanyl on 2021, August 9

