by Jim Hopwood, SVP/Chief Financial Officer and Charles Panicker, Chief Revenue Officer
Not only is the first appointment a critical moment in our patients’ recovery journey, it’s also a critical first step for Revenue Cycle Management (RCM). Collecting upfront all the correct personal information and establishing what insurance coverage and plan they have or if they are self-pay sets the billing cycle in motion, keeping both our budget and quality of care healthy with the least amount of administrative and financial disruptions.
Over the past couple of years, you’ve witnessed our growth and the investments we’re making to upgrade every facet of BHG. As we add more payors and patients, now is the time to fine-tune and modernize our RCM.
What is RCM?
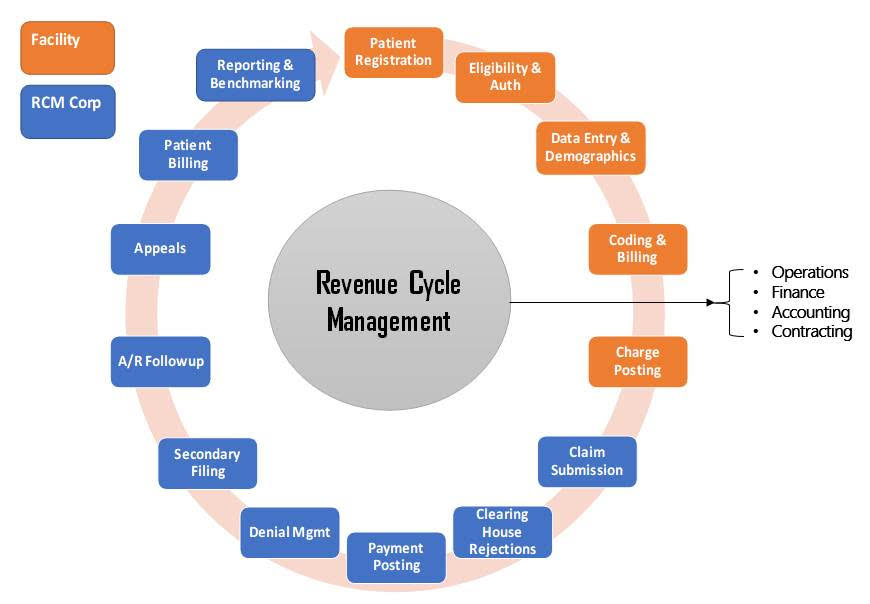
RCM is the process of collecting payments for medical bills to generate revenue for our company, combining patients’ personal data, insurance information and treatment codes with financial billing information.
The Medical Group Management Association’s most recent MGMA Stat poll asked healthcare leaders: “What is your biggest revenue cycle challenge?” A majority (48%) responded “claims payment,” while 23% reported “other” revenue cycle issues, with the top three being denials, prior authorization and staffing issues. Nearly two in 10 (18%) pointed to the capturing and/or sending of claims and another 11% stated “clearinghouse/processing claims.”
RCM is like disaster planning. It helps us stay on top of what’s going in and coming out in a timely manner. It’s the oxygen that moves BHG forward, ensuring we can fund important initiatives that are vital to our mission of restoring lives, strengthening families and rejuvenating communities.
If we make mistakes in the RCM process, we are hamstringing ourselves in all that we’re trying to do like expanding services and implementing new technology, professional development and training, hiring more staff and creating new roles, and making much-needed renovations to treatment centers.
These are common mistakes we experience:
- Coverage. If a patient tells us they have Blue Cross Blue Shield, there are three plan options they could have: commercial, Medicare or Medicaid. If the wrong plan type is entered into our system, that one wrong step can turn our standard 35-day payment cycle into 60 to 90 days or longer.
- Authorization. If a patient comes in and has a plan that requires prior authorization that we didn’t secure before their appointment, that also slows down the revenue cycle. Since we have repeat patients, this misstep only exacerbates the issue. We need more adherence to our monthly eligibility check process to help eliminate this problem.
- Collection. Patients who are self-pay or have high-deductible plans often show up to our treatment centers unable to make payments or unaware of the costs. Once they leave the appointment, their propensity to pay is very low. This slows the collection process down and impacts staff workload.
When mistakes like these happen, it can add up quickly. If multiple centers make these mistakes, we’re looking at a budget shortfall in the millions of dollars.
The RCM process also emphasizes how every job at BHG is important. You’re here for a reason. Without each of you playing your essential part, a bunch of little, big things occur.
So when you think of RCM, think of it as “garbage in, garbage out.” The cleaner the RCM process is at the front end, the cleaner things are going out, providing more revenue predictability so that BHG operations maintains healthy oxygen levels to serve you and our patients.
What RCM improvement means to you
From manual to digital. Currently, patient registration and payment collection are time-consuming, manual and paper-based processes for most of our treatment centers. But good change is coming as we upgrade our SAMMS V5 (substance abuse medication management system) Electronic Health Records (EHR) tool to SAMMS V6. It will be more intuitive than our current system and provide better, faster horsepower that feeds the revenue cycle process “clean” information at the front end. And since this will replace the paper process, we’ll be more environmentally-friendly and saving some trees, too. Be sure to read the Tech Talk story to learn more.
The EHR tool will also help us explore other ways to improve the process for patients and staff. For example, we could provide a self-check-in kiosk where a balance can be paid or we can ensure a private, online portal is available for all patients to complete the registration process before their first appointment.
We are piloting our first fully-digital location at Wellness Knoxville and will be sharing progress reports with you along the way. We started in Tennessee because it’s our biggest region with more payors and RCM complexities to navigate. We aim to make all treatment centers fully digital like Knoxville by the end of 2022.
Improved staff training. Once new payor contracts are established, it’s critical that we provide thorough training to our RCM team, patient registration staff and regional Patient Financial Coordinators (PFCs) and make sure they’re aligned with payors’ expectations.
New regional staff role. To help our teams fine-tune RCM, we are in the process of hiring a National Director of Patient Financial Coordinators. We created this position based on the three pillars of RCM from which we operate: eligibility, authorization and collection.
Perspective from the field

Maury Long, Regional Director – Alabama, said it all boils down to the people you have on your team. When BHG first started acquiring clinics, he inherited four facilities with people who took pride in really understanding the billing process. Two of those original revenue cycle management experts are still with BHG and he appointed them to train all new hires on RCM. Today, he has a total of 12 sites, nine of which accept third party billing and three that remain self-pay for now.
“In my first forecasting call, Jay started talking about third-party billing, Medicaid and Medicare. I had no idea what he was talking about, but I knew there wasn’t going to be another meeting where I wasn’t in the know,” said Maury. “That’s when I realized how big of a factor RCM is to the success of the organization, so I sat with Patty Hoogle, Office Manager for the Tuscaloosa center, and she taught me how to do billing. I learned the entire process and became heavily engaged in monitoring it.”
One of his original staff, Karla Patterson, became a PFC for the region. She recently left BHG to go back to school and get certified in billing and coding.
“I told her to come back to BHG when she finishes school because the RCM team could utilize her help. She said she plans on doing that.”
Most of the centers in Alabama are still doing the manual process, but getting a firm grip on every penny at all times has made his team achieve some of the highest-performing RCM numbers.
Maury said he stays highly engaged in the RCM process and is in constant communication with his team. They have a solid process and rhythm that everyone is committed to, including:
- Weekly monitoring. His centers bill weekly and provide him with a spreadsheet every Friday that includes claims, billing amounts covered by payors, the SOR Grant and patients. “I can see immediately if numbers are down or missing and we can adjust right away. I can also easily see which centers are maintaining their weekly billing and those that are getting behind.”
- Ensures training from the best. Janet Utley was promoted to PFC from one of Maury’s original four patient registration staff. Now, she picks up the slack from what he used to do weekly. “I transferred my mindset to her and now she’s doing the same with our staff. Now, instead of following up with each center, I call Janet for the latest RCM report for our region.”
- Show appreciation. Maury provides incentives to his team to keep the RCM clean. Some sites have lost their patient registration staff and they have to pick up slack, so Maury believes it’s important to demonstrate how much he and BHG appreciates their excellent work.
Maury said it’s crucial to make sure staff understands BHG is not just a counseling facility, it’s also a healthcare operation fueled by the entire Alabama region’s RCM.
“When our centers in Alabama get the updated EHR system, it will free up some time for our staff. All the hard work we’ve done for the manual process will pay off with the new system. We might still use our spreadsheet and do some double checking until we fully trust in it, but our RCM excellence will hopefully be next level.”


